In my opinion, artificial pancreas (AP) technology was the single most important technology of the American Diabetes Association Scientific Sessions this year. There were many papers, posters, and presentations on artificial pancreases and related technologies (such as continuous glucose monitoring, stable glucagon, etc.) Nothing generated more Twitter buzz.
This blog posting attempts to summarize a little of the research presented. There was way too much for me to cover it all, and so this posting gives light coverage to the most important news.
My overall summary is that we are no longer talking about if there will be an AP. The question is: when there will be an AP, and how many APs, and how many different types of technology they will use. I continue to be heartened by:
(a) the progress made by AP research projects over the last few months (and years)
(b) the large number of new companies entering the field
(c) the product roadmap announced by Medtronic as they move their existing partial AP to a full AP.
The AP world is more and more driven by commercial considerations, rather than research considerations, and that is a strong signal that we are close to general availability. (Close meaning years, but not too many of them.)
This tweet summarizes my thoughts, as well:
“Closing the loop is no longer a mystery; it’s not a puzzle. We just have to do it.”
https://twitter.com/eliotmbrenner/status/607536971192377344Second Bi-Hormonal Artificial Pancreas In Development
I recently found out about a second bihormonal AP (in addition to Dr. Ed Damiano's). These researchers are in The Netherlands, and you can read more about it here:
http://www.inredadiabetic.nl/diabetes-product-ontwikkeling/
http://www.inredadiabetic.nl/us/history/
http://www.inredadiabetic.nl/news/
It's a little hard for me to figure out exactly where they are, and I have not found any articles in scientific journals. However, it appears that earlier this year they ran a two day test on one person, and got quite good results. The average BG was 125. Based on that they are hoping to run two clinical trials (called APPEL 4 and APPEL 5) later this year. They hope those trials will used as the basis for European "CE" approval.
Maybe a Third?
They haven't started recruiting yet, but this looks like a phase-II trial for yet a third bi-hormonal artificial pancreas. I'll blog more fully if they start recruiting:
https://clinicaltrials.gov/ct2/show/NCT02379299
Back To Ed Damiano's Bi-Hormonal Artificial Pancreas
Not from ADA, but from another conference, comes this summary of Ed Damino's current status:
http://www.medpagetoday.com/MeetingCoverage/AACE/51551?xid=nl_mpt_DHE_2015-05-16&eun=g118127d0r
But if you want a summary in 140 characters, here it is, from
https://twitter.com/DiabetesMine/status/607298177952321537:
Damiano says #BionicPancreas showing ave BGs of 135-142, which would equate to 6.5% A1C.
[What's not to like!]
Plus there was this good news tweet:
From https://twitter.com/InsulinNation/status/607300794875002882:
Ed Damiano says there is room temperature stable glucagon that stays good for up to a year. Needs FDA approval.
Medtronic's 670G
The Medtronic 670G, as announced, will be an "all but meals" style, single hormone artificial pancreas, available in the United States in April 2017. As far as I know it is the most powerful AP with a clear commercial delivery date. For comparison, the 640G is already available in Europe, but does not prevent "highs," only "lows".
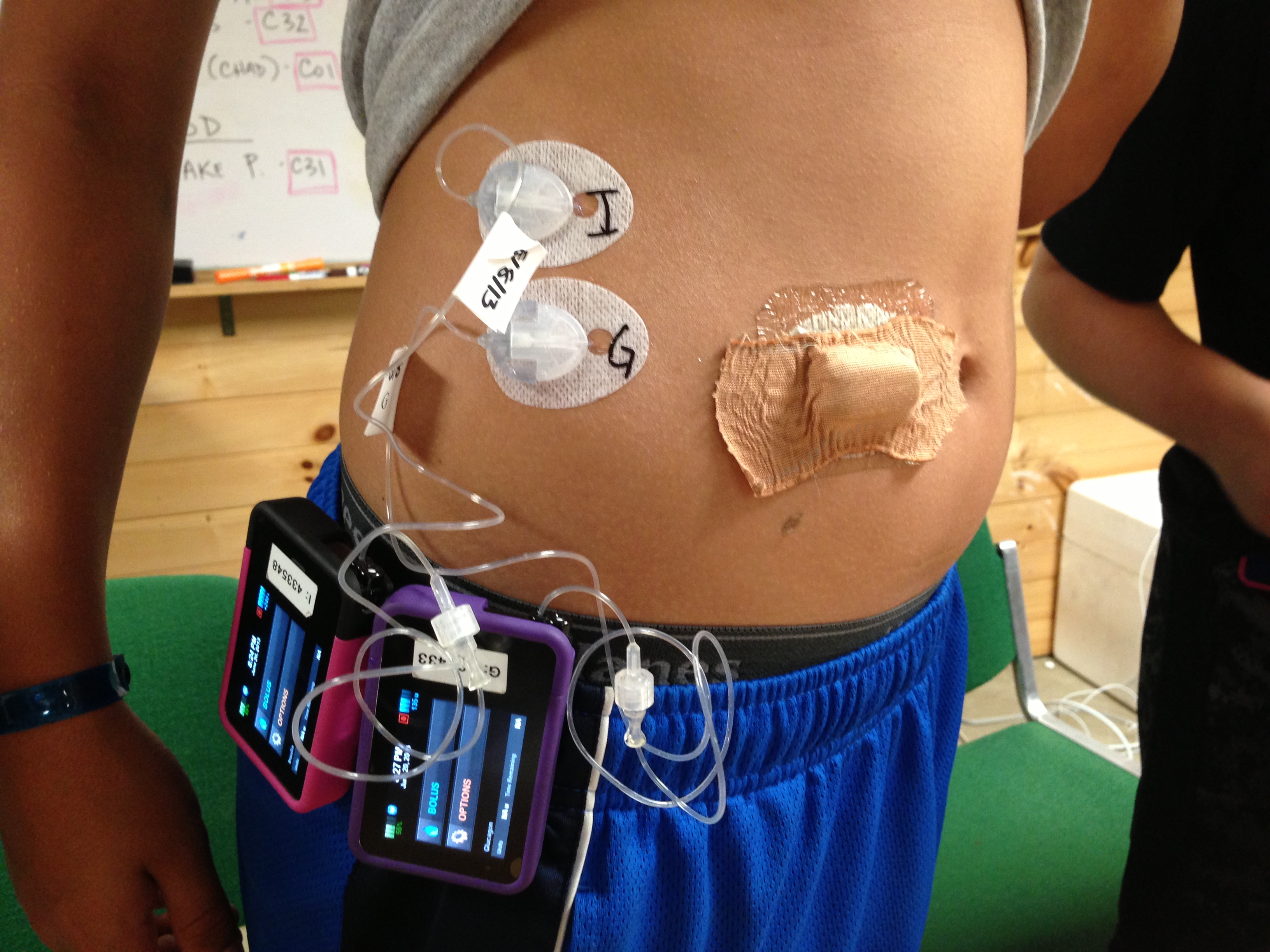
diaTribe interviewed a patient who has used the 670G as part of a clinical trial:
http://diatribe.org/medtronic-minimed-670g-hybrid-closed-loop-exclusive-interview-17-year-old-trial-participant
This is Medtronic's press release summary of results from a 640G study, a 670G study, and some other research they presented at ADA:
http://finance.yahoo.com/news/medtronic-accelerates-path-artificial-pancreas-140201655.html
The current plan is for the 640G to be available next year, and the 670G the year after.
This news resulted in the following tweets (and many more, of course):
https://twitter.com/DiabetesMine/status/607197166193508353
https://twitter.com/DiabetesMine/status/607198339600392192
More General AP News
The following, more cautionary tweets report on other aspects of AP research:
From https://twitter.com/InsulinNation/status/607284169622880256:
During artificial pancreas study, the AP couldn't be used 1 in 3 nights because of tech issues (sensors) or family/health issues.[But I don't know which AP this tweet is about!]
From https://twitter.com/DiabetesMine/status/607284048931770368:
CDE Laurel Messer: Still enough tech issues exist with CGM sensors to impact hoe [sic, should be "how"] closed loop is used in kids and young adults.
From https://twitter.com/InsulinNation/status/607278840193400832:
Predictive pump technology significantly reduced nighttime lows in kids in almost 1000 night study. [But again: I don't know what AP this refers to!]
The following link goes to a summary of one of the ADA sessions:
http://www.saluteh24.com/il_weblog_di_antonio/2015/06/artificial-pancreas-moving-toward-pediatric-use-2015ada-meeting-in-boston.html
Personal testimonial (with graph) of how well an AP works, but I don't know which one! Anyone recognize the screen?
https://twitter.com/DiabeticSisters/status/607709090278699008
Bigfoot Explodes Big (In a Good Way!)
Bigfoot is a one year old company. They had a very successful ADA and generated a lot of "buzz", which this tweet tries to summarize.
From https://twitter.com/diaTribeNews/status/604309757093011456:
@BigfootBiomed acquires Asante pumps! Goal to enter pivotal trial of full #artificialpancreas system late 2016
A "pivotal" trial is industry-speak for a phase-III clinical trial. What they are saying is that they hope to start phase-III trials of an AP next year. That would put them shoulder to shoulder with Medtronic and front running bihormonal research projects. Even if they are overly optimistic, and they actually start those tests in 2017, they are still not that far away from a commercial AP.
But even more promising (to me) is that Bigfoot feels like a tech start up, not a medical device company. It feels like Silicon Valley rather than Washington D.C. I can't tell if that's a marketing strategy or the truth, but if you look at the founders, look at the tactics (reuse the failed carcass of another project), and the strategy: it really does look like the way things happen "out here".
When a company like that can successfully create an AP, it means that APs are technology gizmos, and not medical devices, and technology products can improve much more quickly than medical products. I'm sure the FDA will have something to say about it, but even if Bigfoot is just a 20% step in the direction of Silicon Valley, that's going to "light a fire underneath" some medical device companies.
The following link goes to one diaTribe story, but that story has links to other stories, and you can get the whole saga of how big they've grown, how quickly, and how important that might be:
http://diatribe.org/bigfoot-biomedical-acquires-asante-snap-pump-technology
TypeZero: Yet Another New Company Focused On A Single Hormone AP
And if that were not enough, TypeZero Technologies is yet another new company trying to create a single hormone AP "from scratch". DiabetesMine has a summary article:
http://www.healthline.com/diabetesmine/typezero-tech-closed-loop-commercialization
This is based on AP research done at the University of Virginia which I have reported on before.
Comparison
There was some debate at ADA about which was better: single hormone artificial pancreases, or bihormonal artificial pancreases. My first reaction to this debate was this: who cares? Either one is so much better than what we have now, let the people who like insulin only APs develop those, and let the people who like insulin and glucagon APs develop those, and let the market decide, or maybe let the market decide that there is room for more than one AP technology. I mean some people have cable while others have satellite, why not the same with APs? Have we learned nothing from the death of communism? Let the market decide, as fed by the strongest proponents of each system.
My second reaction to this debate was that it can never be resolved by research. The data we have now is pretty clear: single hormone APs result in average BG numbers about 10 points higher than dual hormone APs (for example mid 130s vs mid 140s). However, dual hormone APs are more complex to manufacture, more complex to operate, and involve the tiny risk of long term, very low dose glucagon (and that risk is unknown, and will remain unknown for years). So some people are going to say dual hormone is 10 points better than single hormone, end of story. But others will say, mucking about with refilling two reservoirs is just not worth 10 points. And neither of these opinions is right or wrong, they are just different. And always will be.
However, even if research cannot answer a question, it can still inform the discussion, and there have been some papers directly comparing the two systems. The following tweet is one summary, but the links to the abstracts below contain more data.
From https://twitter.com/sarhoward/status/608301471529107457:
Haidar: Both single and dual hormone artificial pancreases better than pump for BG control at night, dual better for reducing hypos
http://www.thelancet.com/journals/landia/article/PIIS2213-8587(15)00141-2/abstract
http://www.thelancet.com/journals/landia/article/PIIS2213-8587(14)70226-8/abstract
Joshua Levy
http://cureresearch4type1diabetes.blogspot.com
publicjoshualevy at gmail dot com
All the views expressed here are those of Joshua Levy, and nothing here is official JDRF or JDCA news, views, policies or opinions. My daughter has type-1 diabetes and participates in clinical trials, which might be discussed here. My blog contains a more complete non-conflict of interest statement. Thanks to everyone who helps with the blog.